Am I a good candidate for IVF?
Infertility is much more common than people may think! In the U.S., infertility affects approximately one in eight couples. The causes of infertility may vary between individuals but they can be divided into roughly three major groups—attributes of the female partner, male partner, or a combination of both partners or unexplained. If you’re struggling with infertility, it can be complicated to sort through the array of evaluation tests to figure out which treatment is the right one for you. Fortunately, there is a wide range of fertility treatments for people to consider including fertility medications, surgery, intrauterine insemination (IUI), or even in vitro fertilization (IVF).
Who can IVF treat?
Success with IVF has improved over the years, making it an effective treatment for many people experiencing infertility. Deciding if IVF is right for you depends on your personal situation and your desired outcomes, so speaking with an infertility specialist can help you determine if this is the best treatment option. IVF is often a highly effective option for:
- Women who have tried other infertility treatments and unfortunately have not had success. Women often try inexpensive and less invasive treatments first, such as fertility medications and/or IUI. When these treatments fail, it can be disheartening and emotionally draining. However, in these situations, IVF can be a beacon of hope for those who have had other failed treatments.
- Couples who are >35 years old and have been trying to conceive for more than 6 months.
- Women who have previously chosen to freeze their eggs. Frozen eggs are required to be fertilized through IVF before transferring an embryo into the uterus.
- Individuals experiencing a variety of infertility types, including:
- Tubal Factor—when a blockage in the fallopian tubes prevents sperm from reaching the ovulated egg, therefore preventing fertilization. Since IVF bypasses the fallopian tubes entirely, it is an effective option for women experiencing tubal factor infertility.
- Male factor—when a semen analysis may show significantly low sperm count, low sperm motility, or issues with the shape of the sperm. IVF can address these issues with Intracytoplasmic Sperm Injection (ICSI), in which sperm is inserted directly into the egg.
- Diminished egg reserves/poor quality eggs—couples or individuals experiencing infertility related to a low number of remaining eggs or a history of poor egg quality may choose to use an egg donor. The process of obtaining eggs from a 21-30-year-old donor is achieved through standard IVF.
- Endometriosis
- Couples who choose to use a gestational carrier commonly referred to as a surrogate. Whether it is due to the inability to carry a pregnancy or absence of a uterus, when a gestational carrier is necessary, IVF is the procedure used to create an embryo that can be then transferred into a gestational carrier. This gestational carrier then carries the pregnancy until birth.
IVF Cycle Steps
An IVF cycle can vary based on the personalized protocol for your situation; however, the typical steps include the following events:
- Daily injections of follicle stimulating hormone (FSH) medication is administered to stimulate multiple follicles with eggs inside to grow and develop.
- When the follicles are of appropriate size, an egg retrieval is performed to retrieve them from the ovaries using a needle under ultrasound guidance.
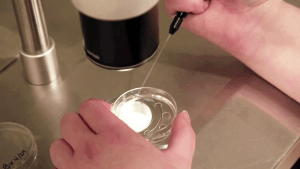
- Insemination of the egg with the partner’s sperm or donor sperm is then performed to achieve fertilization. There are two ways to inseminate the egg—the traditional method (placing sperm around each egg) or ICSI (injecting a single sperm into an egg).
- The new embryos are then cultured in the embryology lab for approximately 5 or 6 days. During this time, they are examined under the microscope for continued growth and graded on their development.
- If a fresh transfer is planned, one or more embryos, per ASRM guidelines, are transferred into the uterine cavity in hopes of implantation and pregnancy.
- Any remaining high-quality embryos can be frozen for additional frozen embryo transfer cycles in the future.
IVF at 40
As a woman ages, the total number of eggs in her ovaries decreases and of those remaining eggs, a higher percentage will contain the wrong number of chromosomes (46). Women are born with all the eggs they will ever have (approximately 1-2 million)—and at menopause, this number likely reaches less than 1,000. Despite the multiple tests available to evaluate a woman’s ovarian reserve, the best indicator of egg quality is age.
For women over 40 years old who are experiencing infertility, the best initial step is an early evaluation. An infertility specialist can perform simple ovarian reserve testing to better help a woman understand her overall ovarian potential. Additionally, other diagnostic tests can be completed to confirm ovulation, whether the fallopian tubes are open, and to evaluate the sperm quality.
After the evaluation is complete, an infertility specialist can interpret all the results to help you determine the most appropriate treatment options—such as standard IVF, minimal stimulation IVF, donor egg, or donor embryo. There are multiple stimulation protocols for IVF and an infertility specialist will work closely with you to personalize your treatment based on your infertility evaluation, personal and medical history, and desired treatment option.
What if I froze my eggs?
Some women may choose to freeze their eggs at a younger age to “freeze time.” As a woman continues to age, the frozen eggs remain the age at retrieval. When a woman is ready to use her frozen eggs, a fertility clinic will thaw them, inseminate the eggs with sperm, and grow them in the embryology lab until the embryos become blastocysts (day 5 or 6 embryos). After thawing the eggs, the embryology lab process is the same as the IVF steps above.
Whether IVF is the right treatment option for you is ultimately a personal decision made alongside the guidance of your infertility physician. Several factors to consider in your decision-making are your diagnosis, age, prior treatments, physical and emotional demands, time requirement, and financial implications. If you are interested in learning more about infertility treatment options, please feel free to schedule a consultation with one of our infertility physicians to discuss your options and develop a personalized treatment plan.
The first step in your fertility journey is meeting with a reproductive physician. Connect with us to schedule your appointment.
[button animation=”none” variant=”1″ icon=”icomoon-home” background=”#739D8B” color=”#FAF7EF” size=”small” url=”/connect/” target=”_blank” ]Connect with us[/button]